I’ve been writing a lot about what happens when I’m not at the hospital…the residue of chemo treatment, if you will. However, it’s 5:45am on Day 5 of Round Four and perhaps about time I shared with you life during treatment, Days 1-6.

Because everything takes three times longer than it should at the hospital, my oncologist and I agreed to start treatment on Monday (Day 1) morning in her office this time around, and then move me into the hospital around noon. This way I would be able to theoretically start the 96-hour infusion by 3 or 4pm, putting the every-24-hour-bag-changes at a somewhat reasonable hour during the day.

So, Monday morning at 8:45am I showed up for my Rituxan infusion with two of my four bags that I bring to the hospital. My backpack has my computer, wallet, DVDs, iPad, and a binder for work from the office. Another bag holds down pillows, a lovely cuddly blanket, stuffed animals, and my hospital slippers…I don’t unpack that bag when I get home, it just lives in the closet between treatments. Once I get to the hospital, I further the “avoid plastic mattress and pillows” process by ordering an egg crate mattress protector. Otherwise, as I discovered during my initial two-week stay, I end up covered in folliculitis from sleeping on a plastic mattress and plastic pillows that don’t breath. I believe that I have mentioned how sensitive my skin is, yes? Michael was going to bring the food bag and the one that holds toys, hospital clothing, soap and toothpaste, chargers, pictures, and a yoga mat later that afternoon (that one is also left in the closet between treatments).

First thing always done at both the doctor and the hospital is a blood draw. Primarily this is used to monitor my white blood count, but as other numbers change it is also used to check on my platelet and red blood counts, as well as various minerals and electrolytes. This Monday, my white blood count was at 1.4, too low to start chemo. Because Rituxan is not chemo (to quote wikipedia, it is a “chimeric monoclonal antibody against the protein CD20, which is primarily found on the surface of B cells. Rituximab destroys B cells, and is therefore used to treat diseases which are characterized by excessive numbers of B cells, overactive B cells, or dysfunctional B cells. This includes many lymphomas, leukemias, transplant rejection, and some autoimmune disorders), it doesn’t affect blood counts, so I received the two-hour infusion, a Neupogen shot to bring everything up, and my doctor sent me home for the night. Shouldn’t do chemo within 24-hours of a blood count stimulator because they just get in the way of each other.

A dose of Rituxan is accompanied by an IV of Benadryl to control any possible allergic reaction (luckily I haven’t had one), so when I got home, I dropped everything on the floor and went to bed. The cats curled up with me, and we had a lovely four-hour nap.
The next morning, Michael and I walk over to the hospital around 7:45 for an 8am check-in. As always, I request one of the four rooms that has a spectacular view of the lake, and this time around I got the best one. Corner room facing north and east, and twice as big as everything else. I literally ran a lap around it when we got in about 8:30. They finally weigh me, take vitals, and draw my blood around 10 (the weight is for chemo dosage, my blood pressure remains low, and my white blood count is up to 25), I get 100mg of Prednisone around 10:30 (yes, that is a HUGE dose), as well as two magnesium pills (apparently I was low), and the chemo process finally starts around 3. It begins with a 15-minute bag of Zofran (anti-nausea), and is followed by the first of four 24-hour bags that looks like tang, and contains Etoposide, Oncovin (or Vinchristine Sulfate), and Hyroxydaunorubicin (or Doxorubicin). Along with this regime, I get saline at 75 mls/hour. At 6pm, I get another dose of Prednisone, and at 10pm I get my night meds (anti-viral etc.).

I see the fellow or hospitalist at least once a day, my own oncologist usually twice a day, and the nurses and techs at least once every couple of hours. Their visits are accompanied by any number of medical students, residents, and other younger people that take one look at the fact that I’m 33 and try not to panic too obviously about the fact that this cancer patient is too young to have cancer. The doctors (who empathize instead of panic, which is frankly lovely) listen to my lungs (so far so good since taking the heart catheter out), my heart (ditto), and my lower intestine. They check my pulses in both wrists and in my ankles, and comment on how everything just keeps swelling and my lower intestine is too quiet. Nurses are in once every two hours (even during the night) to perform a “vesicant” check, which involves pulling blood back up the IV line being used by the chemo. This is done because Doxorubicin burns tissue, which is why it must be infused into a deep vein (I wouldn’t be able to receive this chemo through a normal arm IV because it would burn through the thinner surface vein). The blood check is designed to make sure that it hasn’t burned through my deeper vein or done anything else that would be problematic.

For the first 48 hours, I feel fine. I do work for the office, I putter, I walk laps around the hospital floor, and I generally avoid the bed except when I’m sleeping. After that, things begin to catch up. Vinchristine, ah, shuts down the digestive system, so monitoring that process is ongoing and irritating. The variety of aids they give me to help with that tend to take my system to the extremes, which totally sucks. Further, Prednisone at high doses causes fluid retention. This makes me puffy, which is only truly damaging to my ego, but it also makes the blood pressure cuff incredibly painful. By today (Day 5), I’ve gained 6 kgs since Day 2 (yes, that’s over 12 pounds of fluid in three days — 10% of my body weight). By the time I get home, I lose all of that excess fluid within two or three days, which is another fun process, but no matter how I look at it, I end up feeling like some science experiment that’s gone horribly wrong.

Also by Day 4, I start to get sleepy. Even though nurses are in my room every two hours at night to check the blood return, draw blood at 4am, and check vitals at 6, I still manage to start getting at least 11 hours of sleep at night. This is accompanied by at least two naps a day and general lethargy. At this point, my computer comes out and the tv shows/movies come on. I try to leave my bed just for general mental health reasons, but that doesn’t last for long.

Also by Day 4 the “normal” side effects begin. The metallic taste in my mouth (that usually lasts til about Day 7 or 8) comes back and the tips of my fingers start to tingle/get numb…which has been lasting longer and longer as the number of chemo rounds increases (this is actually a side effect that could be permanent depending on how much damage the Vinchristine does to my nerves and how much they heal between rounds). Plus my hemoglobin levels drop enough to justify a two-bag blood transfusion. This usually occurs during Day 5, in fact I’m scheduled for it this afternoon. This is relatively straight-forward (if I ignore the basic grossness of getting someone else’s blood pumped into me), and usually by the end, I have a lot more energy. Also, my potassium levels start dropping through the floor, so I’ve been getting horse pills of that for the last two days.

By Day 6 (tomorrow, Saturday), the bags of tang are done and I get one final dose of chemo, Cyclophosphamide (this is the truly nasty chemo — itself a carcinogen and the reason my hair fell out in a week), that is administered over an hour, and then I’m released back home! I usually take a nap, my final dose of Prednisone, which causes a total high, and take my puffy face out on the town for one last night before the truly debilitating exhaustion sets in until about Day 11…12…13…this keeps creeping higher as this process continues.

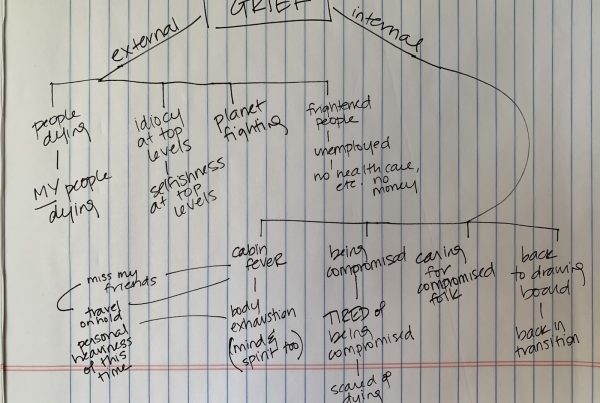
Throughout these six days, I get amazing visits from my amazing friends who bring food or humor or just company. Michael spends the nights with me, and there is a constant stream of incredibly lovely medical staff. However, I’m discovering that the longer this goes, and the more my body and spirit are under attack, the more alone I feel. By its very nature, cancer and treatment for it is a process that can’t really truly be shared. I’m getting support and love and healing energy from all over the world, which is incredible, but at the end of the day, I’m alone. For the first time in my life, I’m beginning to understand the value of support groups. Don’t get me wrong — I’m still me, so the thought of going to one still makes me cringe, but I’m beginning to get it. Thank the gods for my amazing sister.